You probably don't need to follow Covid data anymore, and that's a good thing.
If do you want to track Covid trends, it's not as easy as it used to be.
It’s June 2023. and the end of the U.S. public health emergency for Covid was declared more than a month ago (May 11, 2023). I still have elaborate spreadsheets which automatically pull data from a variety of sources and generate nice graphs. But I’ll be honest: I haven’t looked at Covid data for months and I don’t think you need to either.
If you do want to continue following Covid trends, some of the metrics and data we relied on during the pandemic are no longer available; at least not in the ways they used to be. The metrics we can still easily follow mostly track long-term trends in severe health outcomes, such as hospitalizations and deaths, rather than immediate measures of current spread. Given what the metrics show, I think this is reasonable. I don’t think that the average person, or even hobbyist health data analyst like myself, benefits much from continuing to track Covid metrics on any kind of regular basis.
Covid is not “over,” but the spread of the virus has entered what you could call the “smoldering” stage. Over the last 6-12 months, Covid infections have been at the lowest and most stable level we have seen since the virus was discovered. Tracking Covid metrics on a daily, weekly, or even monthly basis is not likely to inform behavior in a helpful way.
You can be confident that epidemiologists can and will continue to track the spread of Covid infections to watch for significant new variants or waves or anything unusual. They will let us know if or when the situation might change dramatically.
What measure of Covid infections are still available?
Even if you don’t need to watch Covid metrics on a regular basis, it’s still worth being away of how the landscape of data and metrics on Covid is changing. Back when I was regularly posting updates on the virus in Indiana, there were six key Covid metrics I focused on. They were (going from “most responsive” to “slowest to respond”):
Wastewater Concentration
Test Positivity Rate
Cases Identified
Hospital Admissions
Number Hospitalized
Daily Deaths
These six metrics, when combined, provided a relatively good measure of both the rate of spread and severity of Covid infections. Some were less intuitive (such as wastewater concentration and test positivity rate) but effective as early warning systems. Others were more intuitive (such as hospitalization and deaths) but lagged weeks or months behind. In June 2023, do these data still exist and can we track them?
The first three metrics, those most useful for tracking week-to-week changes in infections, are either no longer publicly available (#1 and #2) or else not particularly useful anymore (#3). The final three metrics, those most useful for tracking severe outcomes from infections, are still available. While most of you are probably not interested in the technical details of the availability of these data, I’m going to go through each of these six metrics, looking at the most recent data we have and how the availability of these data have changed.
1. Wastewater Concentration
One of the best measures Covid infections to emerge from the pandemic is viral wastewater concentration, or looking at sewage for the concentration of SARS-CoV-2 virus. It’s a great metric for two reasons: First, it captures an entire sewershed rather than relying on administering tests to individuals, which often go unadministered or unreported. Second, it’s capable of picking up new waves of infections far earlier than other metrics with less reporting delay.
The consistently best source for SAR-CoV-2 wastewater concentration data throughout the pandemic has been Biobot Analytics. They currently track data from over 250 counties across the United States and provide these data publicly in easy to use interactive graphs here. Below you can find a screenshot of the graph for Lake County, IN, which is the second most-populous county in Indiana as well as the county with the longest history of wastewater surveillance in Indiana.
From the graph above, you can see that viral concentration has been steadily falling over the last 12 months. The most recent measure of wastewater viral concentration for Lake County is 82 copies/mL (as of Jun. 7th, 2023), which is one of the lowest levels ever recorded. While it’s difficult to aggregate wastewater data to the state level, the trends and relative levels across Indiana are generally similar to Lake county.
During the pandemic, BioBot Analytics also provided extensive public and freely available downloadable data through GitHub. This was a fantastic resource. However, coinciding with the declared end of the public health emergency, they no longer provide these data, with the last update occurring on May 11th, 2023. They do continue to provide a historical repository of these data.
While downloadable wastewater data is no longer readily available, BioBot Analytics continues to provide up-to-date graphs of the county-level data on their website which you can use to check the current conditions of your county. I have not tried requesting access to downloadable current wastewater data for academic or non-commercial purposes, but based on my experience working with BioBot in the past I imagine this would be a relatively straight-forward process.
VERDICT: Covid wastewater data is still relatively available, but there may be a few more hoops to jump through for full access if you want to do more with the data.
2. Test Positivity Rate
Prior to the widespread availability of wastewater data, the current positivity rate of Covid tests (PCR and/or rapid tests) was our best measure of how our testing capacity was keeping up with current infection levels. Coupled with the next metric (daily new cases) this provided a reasonable proxy for the amount of infections (not just identified cases!) occurring in a region or community. While there are some data available at the federal level, the best positivity rate data for the state came from the Indiana State Department of Health (ISDH).
In March, ISDH decided to discontinue the reporting of testing data (see above) due to the widespread use of at-home tests which almost entirely go unreported. I think this was a totally reasonable decision as this metric outlived its usefulness.
The last recoded levels of test positivity rate I have for Indiana before the data were retired are for 16-18% positivity during the month of January. However, for the reasons above, this is difficult to interpret as anything other than “we’re doing less official testing than we used to,” which isn’t a particularly helpful conclusion.
VERDICT: Positivity rate data was a useful tool at getting around the flaws of official identified cases data, allowing us to get a rough approximation of how quickly the virus was spreading. With official recorded testing plummeting, as well as better metrics of spread rate like wastewater data, it was time to retire these data.
3. Cases Identified
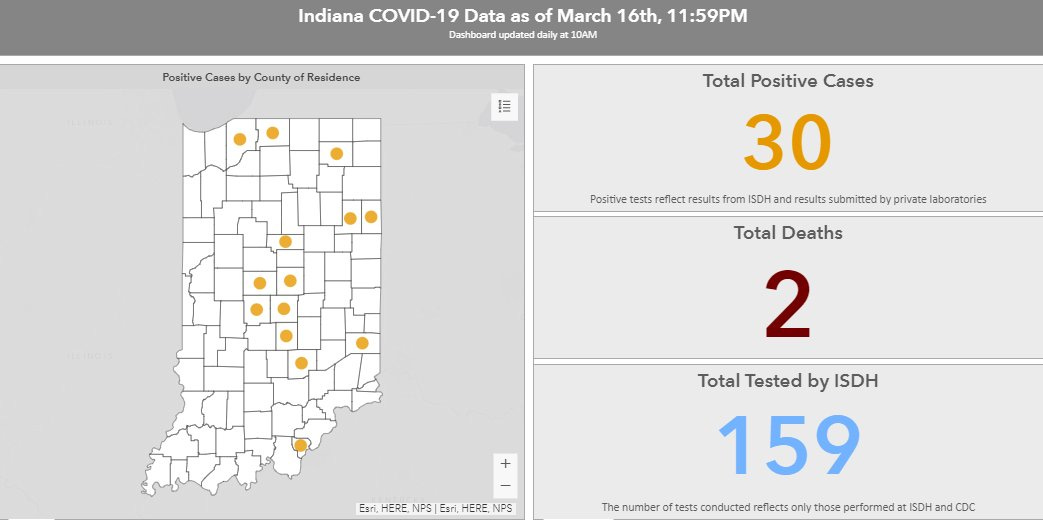
The earliest and most basic metric available for tracking Covid in Indiana was the daily number of new cases identified. For nostalgia’s sake, below is a screenshot of what the ISDH Covid-19 dashboard looked like back on March 16th, 2020 when we had just 30 total reported cases. Today the ISDH dashboard reports over 2 million confirmed infections and reinfections.
Early on, cases confirmed or identified through official testing was the most meaningful metric, because it represented actual confirmed cases of a novel virus you could point to. However, over the months and waves of infection that followed, the metric became harder to interpret. In order for a confirmed case to be recorded, it required that official testing was available (it often wasn’t) and that individuals who knew they might be infected chose to get tested (they often didn’t). Once over the counter at-home rapid tests became widely and readily available (Winter 2021), official testing fell dramatically and was mostly limited to healthcare facility settings.
Today, ISDH continues to report official positive test results weekly. Below you can find a graph of average daily new cases identified in Indiana (note the log scale). As of last week, we were averaging 78 confirmed cases per day in Indiana. This is the lowest daily new cases since the very first weeks of the pandemic. The low case numbers can be attributed almost entirely to low infection rates, but at least some is due to reduced testing. While the state still reports this case data, while testing rates continue to decline, without accompanying data on tests administered, cases are a difficult metric to interpret and probably undercount infections far more than earlier in the pandemic.
VERDICT: Covid cases officially confirmed and reported by the state will always be an important metric, particularly once testing levels stabilize to whatever the long-term testing rate will be. For now though, these data are of limited use and can’t really be compared with levels from 2020-2022.
4. Hospital Admissions
These last three metrics capture measure of severe health outcomes that follow from being infected with Covid. This first, hospital admissions for Covid, captures how many Hoosiers require serious enough medical care to be admitted to a hospital on a given day during a week. Until we have more nuanced measures for things like Long Covid (PASC) this is likely the best measure for the severity of infections from the SARS-CoV-2 virus.
As of the first week of June, Indiana admitted an average of 68 people per day for Covid. This is the lowest level recorded since the data were first collected. This is the best evidence we have that not only are infections with the SARS-CoV-2 virus declining, but the severity of these infections is also falling.
VERDICT: This federal data continues to be available at the state level for now. While it is slower to respond to changes in spread and infection rates, it’s ultimately a more relevant metric than cases as it tells us a lot about the severity of infection.
5. Number Hospitalized
Another important measure of the severity of Covid outcomes is the number of patients currently hospitalized. During the peak of the pandemic, this was an important metric related to the capacity of our healthcare system. As of the first week of June, there were 141 patients hospitalized for Covid in Indiana. This is very close to our record low (which was set at 137 the week before) and a tiny fraction of the thousands we had during the peak of the winter waves (the record high was 3,402 patients during Dec. 2020 to be precise).
VERDICT: This federal data continues to be available at the state level for now. While this is another way to track the severity of infection, it’s most useful to monitor how close our healthcare system is getting to being overwhelmed. With Covid infections (and the severity of those infections) at record low levels, the overwhelming of our healthcare system is something we can worry less about.
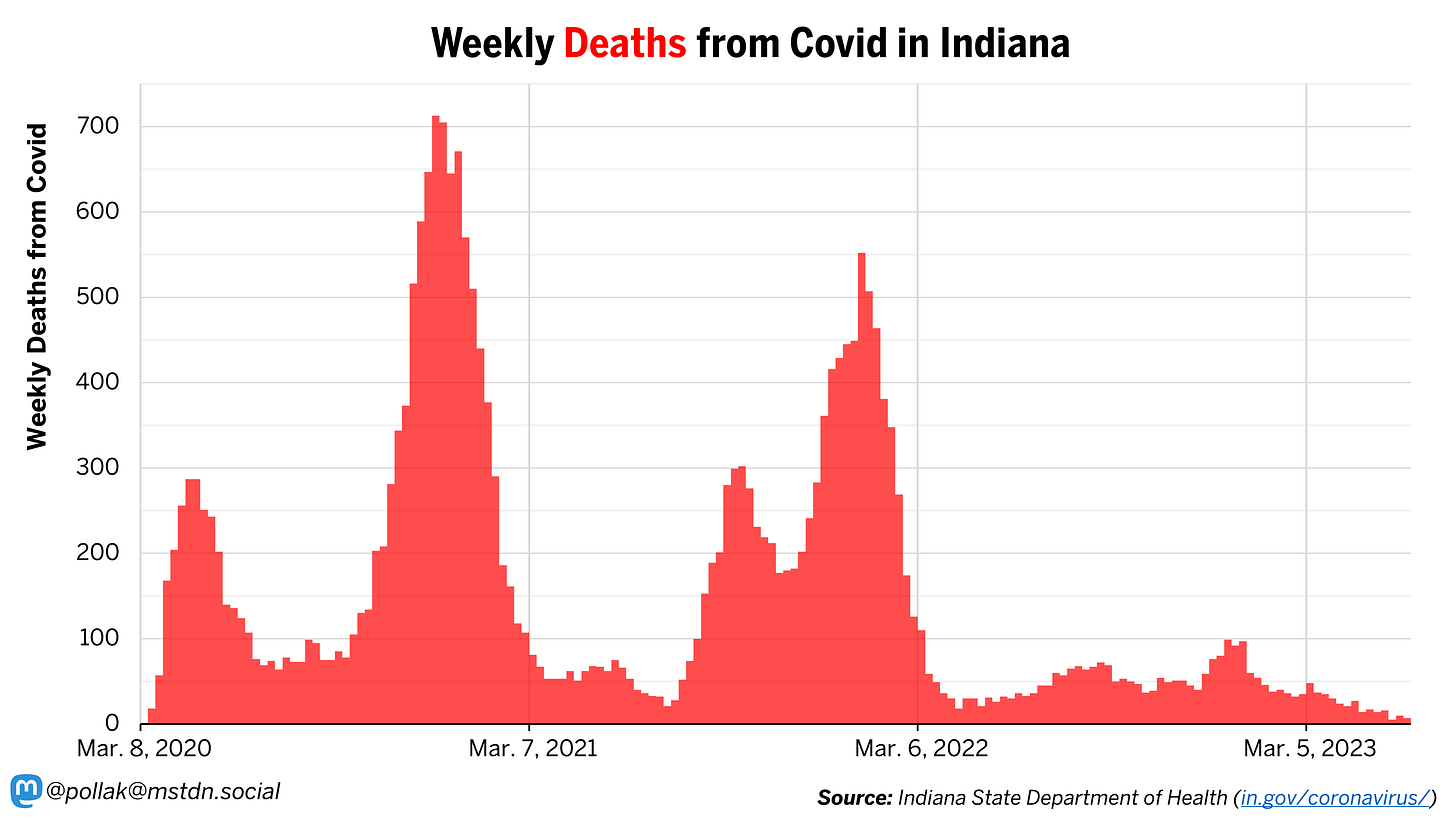
6. Daily Deaths
Finally, we reach what is very likely the single most important metric when it comes to tracking the SARS-CoV-2 virus: deaths from Covid in Indiana. Thankfully, ISDH continues to report new deaths on a weekly basis. The graph below shows weekly deaths from Covid in Indiana. Over the most recent seven weeks, the state has seen an average of 12 deaths per week from Covid, or roughly five deaths every three days, which is a record low by a wide margin. For contrast, during the worst of the pandemic (early Dec. 2020) the state was reporting five deaths from Covid every 70 minutes(!).
Deaths from Covid are a very coarse measure of the severity of SARS-CoV-2 infections. Hopefully, this metric will become less and less relevant as we continue to reduce the infection fatality rate of the virus through protection from vaccination and previous infections as well as continued improvements with treatment and care.
VERDICT: The state continues to provide this data on a weekly basis and it is arguably the most important metric for capturing the severity of SARS-CoV-2 in Indiana.
The Bottom Line
The quality and availability of data and metrics for tracking Covid (i.e. the impact of the SARS-CoV-2 virus) are declining, but this is mostly a reflection of the decline in the spread and severity of the virus. Every metric we have currently points to a steady decline in infection rates and severity of illness from this virus over the last 12 months or longer. Given this, I don’t think the average person, or even hobbyist health data analyst like myself, should feel the need to track or pay attention to Covid metrics on any kind of regular basis. The metrics and data tools developed during the pandemic continue to exist and are being monitored by epidemiologists. For most of us, knowing that the SARS-CoV-2 virus is out there smoldering is helpful, but we’re at a point where short-term changes in virus spread are unlikely to significantly affect decision making anymore.
As the spread and severity of the virus continues to subside, it makes sense to retire, or publish less frequently, data that we previously relied on to inform our decisions. These resources can be better spent elsewhere, such as tracking Long Covid (PASC) or other viruses and health concerns entirely. Long-term I do hope that at the federal level (HHS in particular), we continue to have access to regular data on admissions and patients in hospitals for Covid and at the state level, regular reports on new cases and deaths from Covid. While there is still much uncertainty surrounding the SARS-CoV-2 virus, particularly when it comes to long-term health consequences, for most of us, tracking the immediate spread of the virus is becoming less of an important part of our daily life. I plan to keep my elaborate spreadsheets around in case I need them again, but I suspect they will mostly be gathering digital dust.